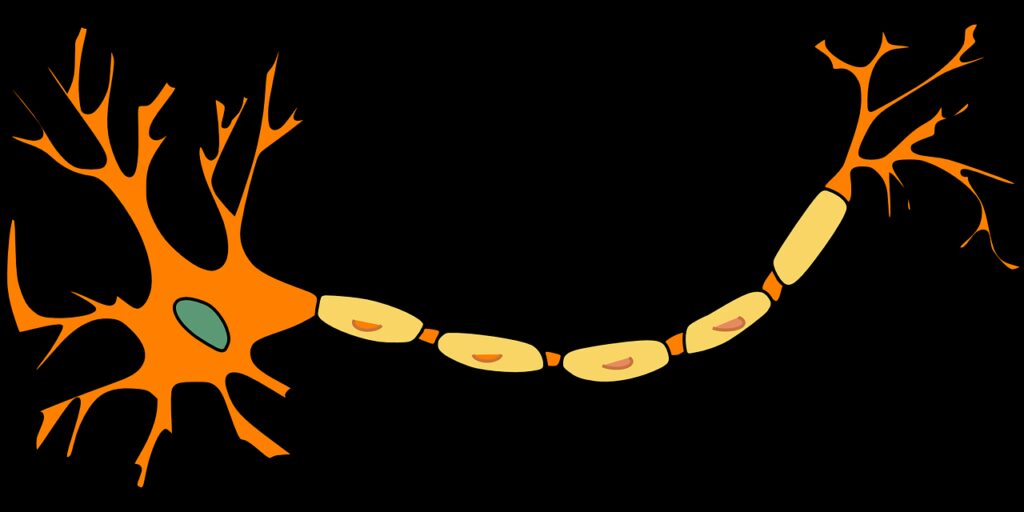
Nerve cells, also known as neurons, communicate with one another by means of chemicals called neurotransmitters, which are released by one neuron and interact with receptors on another neuron.
The action of neurotransmitters is terminated by being taken back up into the neuron that released them (known as ‘re-uptake’).
Depression is thought to be associated with low levels of certain neurotransmitters, particularly noradrenaline (also known as norepinephrine) and serotonin (also called 5-hydroxytryptamine or 5-HT).
Most antidepressant drugs are therefore designed either to prolong the effects of the neurotransmitters by blocking their re-uptake into the neuron that released them or to increase the amount that is accumulated in that neuron and so available for release.
Most types of neurotransmitters have actions at several different sites in the brain, and in other parts of the body, as well. This means that drugs that interfere with their actions will have side effects caused by the effect of the same type of neurotransmitters in other areas.
As we learn more about the specific actions of different neurotransmitters, we can classify their receptors into different subtypes, depending on what response they trigger; for example, noradrenaline receptors are classified as alpha and beta receptors. Many people are familiar with the term ‘beta blockers’ – these drugs block beta receptors and therefore reduce the effect of noradrenaline at these sites.
In designing new antidepressants, the aim is usually to make the drug target the brain receptors thought to be directly involved with depression, to avoid changing the action of the neurotransmitter at other sites which may give unwanted side effects.
