
Admin
Consent to Medical Treatment

This blog post was written to answer some of the more common questions concerning consent to medical treatment. It should be helpful to users of mental health services, their relatives and friends, as well as to service providers working in the statutory and voluntary sectors. It is not, however, a substitute for a statement of the law or for legal advice. We will discuss:
- Introduction
- What is Consent to Treatment?
- How Much Information Should I Be Given About the Treatment?
- Who Can Consent to My Treatment?
- What Does ‘Capacity’ Mean?
- What Is An ‘Advance Directive’?
- Will An ‘Advance Directive’ Enable Me to Prevent Treatment I Do Not Want?
- Can I Be Forced To Accept Treatment?
- What is Meant By ‘Immediate Danger’?
- What Does The Mental Health Act 1983 Say About Consent To Treatment?
- Can I Be Treated Without My Consent?
- How Long Will This Last?
- What Will The SOAD Do?
- What If I’m Treated Without My Consent?
- Can I Challenge Forced Treatment Under The European Convention?
- Can I Be Forced To Take Medication When I Am Living In The Community?
- Legal Definitions
Introduction
Public funding may be available to pay for professional advice from a solicitor. It is means-tested (it depends on your income and savings) for most purposes, but not for appeals to the Mental Health Review Tribunal, which are free. Alternatively, you could get in touch with the Law Society, whose website has a list of solicitors suitably experienced to advise on the Mental Health Review Tribunal. Each hospital ward should also hold a list of local mental health solicitors.
Legal terms, as they appear in the Mental Health Act 1983, are printed in bold when they are used for the first time in this booklet (subsequently, they appear in ordinary type). Some people find these terms inappropriate, even offensive, but they are used here for the sake of legal accuracy. (Any definitions appear under Legal definitions.) To keep the guide as straightforward as possible, we have kept technical terms to a minimum and have summarised the effects of the law and good practice, where appropriate. Where we use section numbers, they are from the Mental Health Act 1983.
What is Consent to Treatment?
Before anyone can touch you, they need a lawful justification, otherwise, it is an assault or a battery. The principle is even more important if the ‘touching’ is a major operation, such as open-heart surgery. This applies to all medical treatments, including those for mental health problems. Consent to medical treatment is one such justification and must usually be obtained before any treatment is given. Consent can only be meaningful if a full explanation of the treatment has been given.
How Much Information Should I Be Given About the Treatment?
You should be given all the information you need to enable you to make a decision. This will include what the treatment is, what it will achieve, any likely adverse effects, what will happen if the treatment is not given and what alternatives there are. Doctors are under guidance to encourage you to ask questions and to answer them fully.
Who Can Consent to My Treatment?
Usually, if you are over 18 years old, only you can consent to your medical treatment. There are exceptional circumstances, such as being detained under the Mental Health Act 1983, when treatment can be given to adults who are not consenting.
If you are under 18 years old, the law is complex and it is best to seek specialist advice. It may be that you can consent on your own behalf, but this does not necessarily mean you have the same right to refuse. Others, such as your parents, guardian, the local authority or the court, may be able to consent on your behalf.
What if I Do Not Want the Treatment that is Being Proposed?
If you are an adult and have the capacity to consent, normally you are quite entitled to refuse treatment (although this may not apply if you are detained under certain sections of the Mental Health Act 1983.
It is often as well to discuss concerns you have about treatment with your doctor, making sure they know what it is about the treatment you object to. You can always ask for a second opinion to discuss the treatment proposed. Your GP can arrange this, or your consultant psychiatrist if you have one.
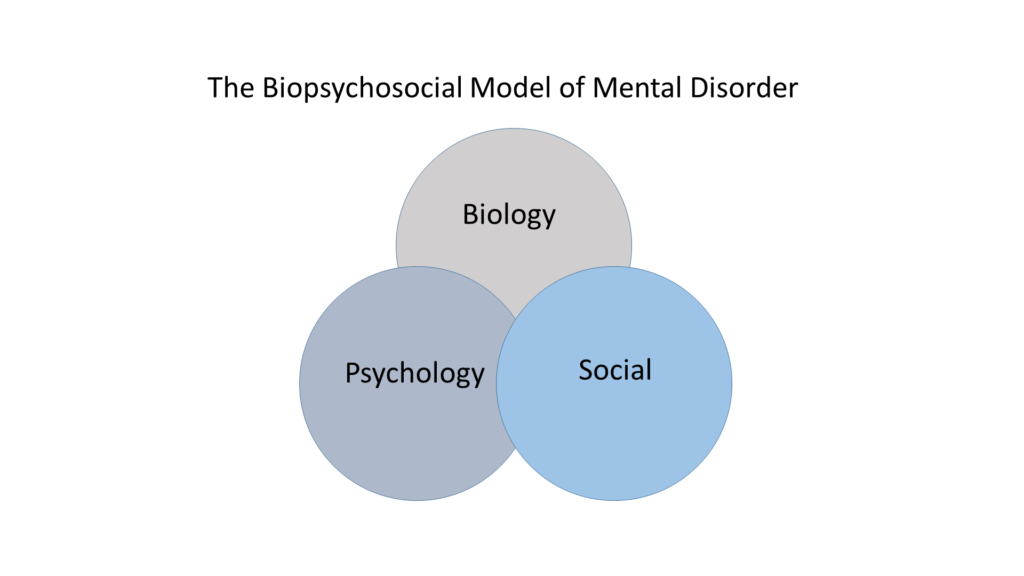
What Does ‘Capacity’ Mean?
Generally, the law presumes you are able to make decisions for yourself. If it is thought you may not be able to decide on a particular issue, for example, whether you want a certain treatment or not, the law uses a test for this ability, which is in three parts:
- Are you able to understand and remember information about the treatment?
- Do you believe that what you are being told is true?
- Can you weigh up the pros and cons of accepting or refusing the treatment, and make a decision based on that?
If a person fails any of these tests, then they will be ‘incapacitated’ and cannot give valid consent. The law then allows the treatment to be given, if it is in the best interests of the patient, according to the principle of ‘necessity’. That means that the treatment must be necessary to ensure health and welfare or prevent deterioration, and also that other doctors would agree that treatment was the correct one. For certain major treatments, the court would have to approve.
The consultant in charge of the person’s care makes the decisions about a person’s capacity and treatment. Good practice requires them to discuss the issues with other professionals involved in the patient’s care, with their family and with close friends, so that all relevant information can be obtained.
The law states that the treatment cannot be given if the patient has made an ‘advance directive’ stating clearly that they did not want the treatment. But this might not apply if the treatment is being given under the Mental Health Act 1983.
What Is An ‘Advance Directive’?
These are sometimes called ‘living wills’ and are a way of controlling what medical care you receive when you are no longer able to make decisions. There are no rules about what an ‘advance directive’ has to look like. It must be made when you have the capacity to do so and may be written or verbal.
Will an ‘Advance Directive’ Enable Me to Prevent Treatment I Do Not Want?
Yes, as long as other legislation does not overrule it and your situation has not changed significantly since it was made. In limited circumstances, the Mental Health Act 1983 can be used to treat a person, even if they have made an advance directive objecting to the treatment.
Can I Be Forced To Accept Treatment?
It may be that you are at home or on a psychiatric ward and feel that you are being pressurised into consenting to medication, for example. You are entitled to refuse and no undue pressure should be placed on you. You should be aware, though, that whilst every effort should be made to obtain your consent to any proposed treatment, the law does allow treatment to be given without your consent in three instances:
- when a person is incapacitated (see above)
- if there is an immediate danger to the patient or someone else (see further down)
- when the special rules in Part IV of the Mental Health Act 1983 apply (see further down).
In view of this, you have to decide whether it is likely that any of these powers will be used if you refuse treatment. If you feel these powers are being used as threats to coerce you into consenting when you would not otherwise do so, seek independent advice and use the complaints procedures.
What is Meant By ‘Immediate Danger’?
If a person is acting in a way that is immediately and seriously dangerous to themselves or others, the law allows health professionals to give a limited amount of treatment, without obtaining consent first.
This is to alleviate the immediate situation and it cannot be continued beyond that time, or if the patient refuses to consent. If the consultant in charge of your care wishes to continue any particular treatment, and you are not consenting, then they must consider an assessment to decide whether the use of the Mental Health Act 1983 is appropriate.
What Does The Mental Health Act 1983 Say About Consent To Treatment?
A treatment plan can be imposed if you are detained under some sections of the Mental Health Act 1983.
The following rules are in Part IV of the Mental Health Act 1983:
- If you are detained under any of the following sections, your consent should always be sought, as above. But if you do not consent, then treatment can be given anyway (sections 2, 3, 36, 37, 38, 45A, 47 or 48).
- If, however, you are detained under the ‘emergency’ sections (4, 5 and 136), which are designed to hold you in hospital till you are properly assessed, the rules under Part IV do not apply, and you have the same rights as if you were not detained.
Can I Be Treated Without My Consent?
Medical treatment for mental disorders can be given to you whilst you are detained (section 63). The definition of medical treatment used here is very broad. It includes most treatment and care available on a psychiatric ward, such as nursing care and medication, and even physical restraint or force-feeding. It also encompasses treatment that could not be given without your cooperation, such as talking treatments.
It has not yet been decided, in law, whether physical treatment, such as blood tests (associated with some psychiatric drugs), can come within the definition. If it is proposed to give you such treatment, and you object, then seek legal advice as soon as possible.
How Long Will This Last?
Treatment given under the Act generally does not have a time limit. It can be given without your consent for as long as you are detained under section. If you want to challenge your continued detention in hospital you can.
There are three important exceptions:
- Psychiatric drugs can be given to you for three months, but then an independent doctor must consider whether you should continue to receive them, or not (section 58). This doctor is sent by the Mental Health Act Commission (MHAC) and is called a Second Opinion Appointed Doctor (SOAD).
- If you do not consent to electroconvulsive therapy (ECT), it cannot be given until a SOAD has been appointed to consider whether the treatment should be given, or not (also section 58). However, in emergencies, treatment can be given before the SOAD arrives (section 62).
- In rare situations, a doctor may propose some form of psychosurgery (lobotomy, leucotomy or implants). Such treatment cannot be given without your informed consent and a second opinion that it is in your best interests (section 57).
What Will the Second Opinion Appointed Doctor (SOAD) Do?
The SOAD will assess you and discuss your health with your Responsible Medical Officer (RMO), with a nurse involved in your care and with another professional involved in your care who is not medically trained, such as an occupational therapist or social worker.
Your RMO must provide the SOAD with a specific treatment plan, including details of medication or numbers of ECT sessions as is felt appropriate. The SOAD will decide whether you are able to consent, or not, and whether, in her or his opinion, the treatment should be given. He or she will then need to record this decision on a special ‘certificate’. Their decision is a personal one and must be independent, but research shows the SOAD is likely to agree with what your RMO proposes.
If the treatment is medication, this certificate will permit treatment to be given to you for as long as you are detained under section.
For ECT, a limited number of treatment sessions will be specified, and when this number is reached, the SOAD must return to make a fresh assessment.
What If I’m Treated Without My Consent?
You should make it clear to your RMO that you object to the medication, and explain your reasons. You can consider complaining under the hospital complaints procedure. The ward staff should help you to do this or to contact an independent adviser, such as the Citizens Advice Bureau or a solicitor. In England, it may be useful to contact your Local Patient Advice Service, which may be able to refer you to your nearest Independent Complaints Advocacy Service (ICAS).
You can also write to the Mental Health Act Commission (MHAC) since they will receive regular reports from your RMO about your health. You can ask that they send the SOAD back to see you. If the MHAC does this, it will most likely be the same doctor.
Since the legal force of a certificate for medication runs whilst you are detained, you should obtain legal advice about seeking discharge from the section under which you are detained.
Can I Challenge Forced Treatment Under The European Convention?
Forced treatment potentially violates a person’s right to respect for his or her private life Article 8 of the Convention). However, this right is not an absolute one. Treatment that your doctor says is ‘therapeutically necessary’ will not violate Article 8, unless you can show that the harm to you from receiving the treatment significantly outweighs the benefit the psychiatrist claims you will get from it. This is normally very difficult.
Can I Be Forced To Take Medication When I Am Living In The Community?
You cannot be compelled to take medication in the community. This is the case even if you are subject to supervised discharge. However, you may decide you have little choice about continuing to take your medication, for example:
If you are still on section, and your RMO has given you leave from the ward, she or he can revoke it at any time and require you to stay on your ward (section 17). Your RMO should not do this simply because you stop taking medication, but it may well lead them to a review of your health, and a consideration of whether leave should continue.
Similarly, if you have been conditionally discharged from the hospital and are subject to supervision in the community, the Home Secretary may review your case, and has the power to recall you to the hospital, if you are becoming a risk because you cease taking medication.
If you are discharged from being sectioned, you do not have to take medication. If you stop, though, an assessment may be organised to decide whether you should be readmitted to a hospital, possibly under the Mental Health Act 1983.
Legal Definitions
Capacity – the ability to understand, remember and believe treatment information, weigh up the pros and cons of accepting treatment and make a decision based on that.
European Convention on Human Rights – fundamental legal principles, which must be applied to any situation involving public authorities, such as the NHS or social services.
Hospital – for the purposes of this blog post, this includes a private hospital and any accommodation provided by a local authority and used as a hospital.
Medical treatment for mental disorder – includes nursing and also includes care, habilitation and rehabilitation under medical supervision' (section 145).
Mental disorder – ‘mental illness, arrested or incomplete development of mind, psychopathic disorder or any other disorder or disability of mind' (section 1). There are four forms:
- mental illness, which is not defined
- mental impairment, which means ‘a state of arrested or incomplete development of mind (not amounting to severe mental impairment) which includes significant impairment of intelligence and social functioning and is associated with abnormally aggressive or seriously irresponsible conduct on the part of the person concerned’
- severe mental impairment, which means ‘a state of arrested or incomplete development of mind, which includes severe impairment of intelligence and social functioning and is associated with abnormally aggressive or seriously irresponsible conduct on the part of the person concerned’
- psychopathic disorder, which means ‘a persistent disorder or disability of mind (whether or not including significant impairment of intelligence), which results in abnormally aggressive or irresponsible conduct on the part of the person concerned’.
Mental Health Act (MHA) 1983 – the main Act of Parliament governing patients' rights in psychiatric services.
Mental Health Act Code of Practice – the statutory Code guiding professionals in the use of the Mental Health Act 1983.
Mental Health Act Commission (MHAC) – the government agency responsible for the welfare of detained patients.
Mental Health Review Tribunal (the tribunal) – an independent panel, which decides if a patient should remain subject to detention under the Mental Health Act 1983.
Responsible Medical Officer (RMO) – the doctor responsible for the care of a detained patient.
Second Opinion Appointed Doctor (SOAD) – an independent doctor who may authorise treatment under the Mental Health Act 1983.





Responses